Orofacial Pain, TMJ Disorders & Dental Sleep Medicine Specialists
Healing the Source, Not Just the SymptomsTMJ vs TMD
TMJ stands for Temporomandibular Joint, TMD is Temporomandibular Joint Disorders. The Temporomandibular Joint (TMJ) Association states that estimates range from 10 million to over 35 million people in the United States are affected by TMJ disorders (TMDs) at any given time.
Common Symptoms of Temporomandibular Joint Disorders:
- – Headaches, earaches, and facial discomfort
- – Crunchy sensations or jaw dislocation
- – Clicking, popping, or cracking sounds in the jaw
- – Jaw locking or difficulty opening/closing the mouth
- – Pain or tenderness in the jaw, face, or around the ears
- – Ringing, fullness, or hearing loss in one or both ears
Why See Us?
Symptom changes may signal TMJ disc displacement or evolving joint health. Early assessment can prevent further joint damage and complications. Persistent symptoms may indicate underlying TM joint or TMJ disc issues.
Don’t wait for your patients’ symptoms to worsen. Let our U.S. residency-trained TMJ Specialists help consult and restore your patients’ comfort and jaw function!
 The temporomandibular joint is one of the most active joints in the body. It is involved in a wide range of daily activities, and as such, it gets used a lot. Estimates vary slightly, but generally, a person uses their TMJ between 2,000 and 3,000 times per day.
The temporomandibular joint is one of the most active joints in the body. It is involved in a wide range of daily activities, and as such, it gets used a lot. Estimates vary slightly, but generally, a person uses their TMJ between 2,000 and 3,000 times per day.
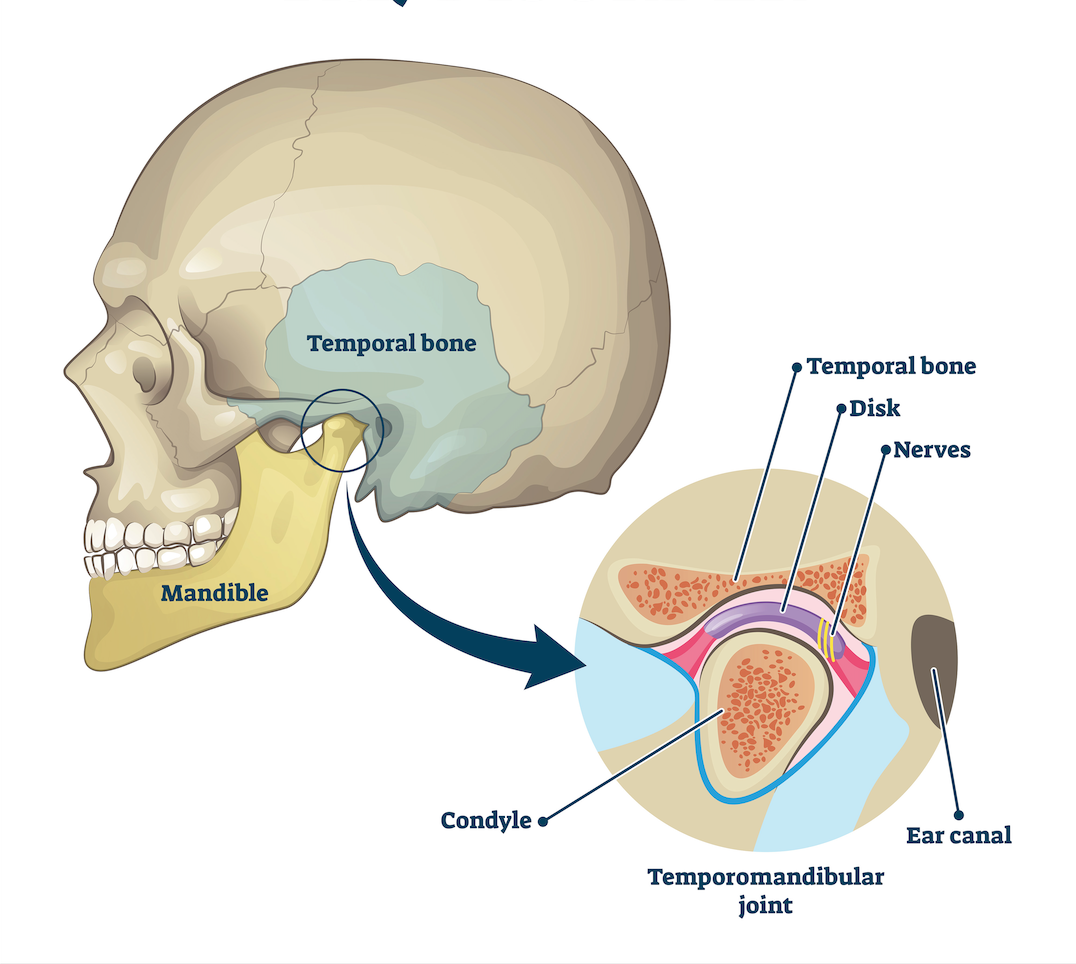
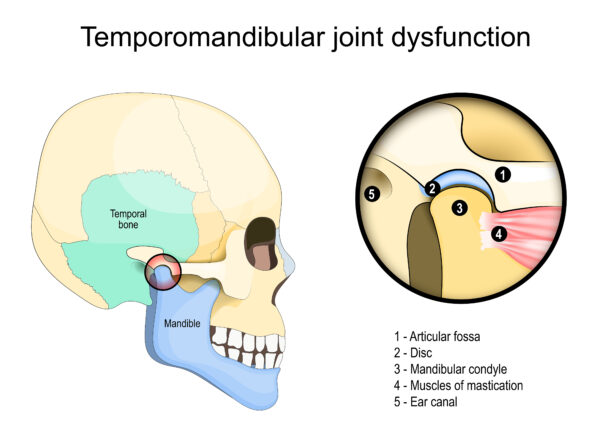
Temporomandibular Joint Disorder (TMD) is a complex condition that affects the jaw joint and surrounding muscles. The lower jawbone (mandible) and the temporal bone of the skull are connected by the temporomandibular joint (TMJ), which acts as a hinge. These joints control jaw movement and are situated on both sides of the head, just in front of each ear. They collaborate with muscles to do so. They enable essential functions like chewing, talking, and opening and closing the mouth.
TMD is a condition in which one or both joints are dysfunctional. This can be caused by structural problems, muscle problems, or lifestyle factors. The disorder affects the muscles and joints that move, causing pain and discomfort. While mild cases may resolve on their own, more severe or persistent TMD often requires professional treatment to manage symptoms and restore proper jaw function.
 Routinely, jaw movements include chewing, talking, yawning as well as mouth breathing and snoring. The National Institute of Health estimates 10 million Americans are afflicted with some form of TMD capable of developing into significant, long-term problems.
Routinely, jaw movements include chewing, talking, yawning as well as mouth breathing and snoring. The National Institute of Health estimates 10 million Americans are afflicted with some form of TMD capable of developing into significant, long-term problems.
The prevalence of TMD is estimated to be between 5% and 12% of the population. A systematic review and meta-analysis found an overall prevalence of approximately 31% for adults/elderly.
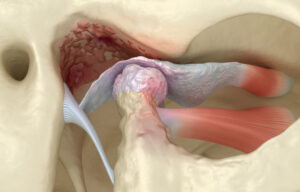
People suffering from TMD usually have symptoms that include clicking, popping, dislocating, cracking, crunchy sounds in the TMJ area, or jaw locking. This may be due to the TMJ disc that cushions the joint and might be dislocating or getting stuck. Sometimes people complain of ringing/fullness in one or both ears and may experience hearing loss.

Clinical Evidence based TMJ/TMD Management that we routinely provide includes:
Self-Care
Resting the jaw, soft foods, stress management, good posture, and TMJ awareness routinely help alleviate some of the symptoms. A simple consultation with a specialist helps.
Medications
These range from OTC NSAIDs like Ibuprofen or Acetaminophen to various muscle relaxants and other prescription medications as well as short term corticosteroids. These are typically prescribed for short-term relief only.
TMJ Splints
There are custom made oral appliances that help in realigning your jaw and preventing jaw clicking/popping or locking. There are many types and the diagnosis of TMD is particularly important for the correct management of your condition. Studies have shown that many times patients wear the wrong appliance, including nightguards, that makes the TMJ pain typically worse after being worn for only a few weeks.
Physical Therapy
We work with therapists to educate about your condition and help improve jaw mobility and range of motion. These may include manual therapies such as massaging, stretching, as well as Transcutaneous Electric Nerve Stimulation. At times we recommend Myofunctional Therapy, a specialized form of physical therapy for the muscles of the face, mouth, tongue, and jaw that aims to address the underlying muscular imbalances and dysfunctional habits contributing to TMJ pain and dysfunction.
Injections
There are a variety of injections that TMJ specialists use that have shown great results depending on the TMJ issues. Common ones include:
Trigger Point Injections:
Injecting medication to break the muscle knots in your jaw muscles. Detailed information is on our Myofascial Pain page.
Botulinum Toxin Injection, e.g., Botox/Xeomin:
Botox and Xeomin, commonly known as wrinkle reducers, are also powerful medical treatments for various functional problems, not just cosmetic ones. These include migraines and chronic headaches, overactive bladder, muscle spasticity, and increasingly, jaw muscle pain (such as severe teeth grinding and TMD, or Temporomandibular Disorders). For headaches, the injections work by blocking pain signals and relaxing the muscles. The medication is a neurotoxin that works by being injected into the muscle, temporarily blocking nerve signals to reduce hyperactivity. This controlled relaxation helps stop muscles from overworking, which breaks the cycle of chronic jaw pain. While the naturally-occurring toxin can be dangerous in large amounts (causing botulism), the tiny medical dose used is safe and effective. Patients typically feel the effects within a few days to a couple of weeks, with relief generally lasting about three to four months. If your symptoms are severe, your doctor may recommend more frequent injections.
Regenerative Injection Therapies:
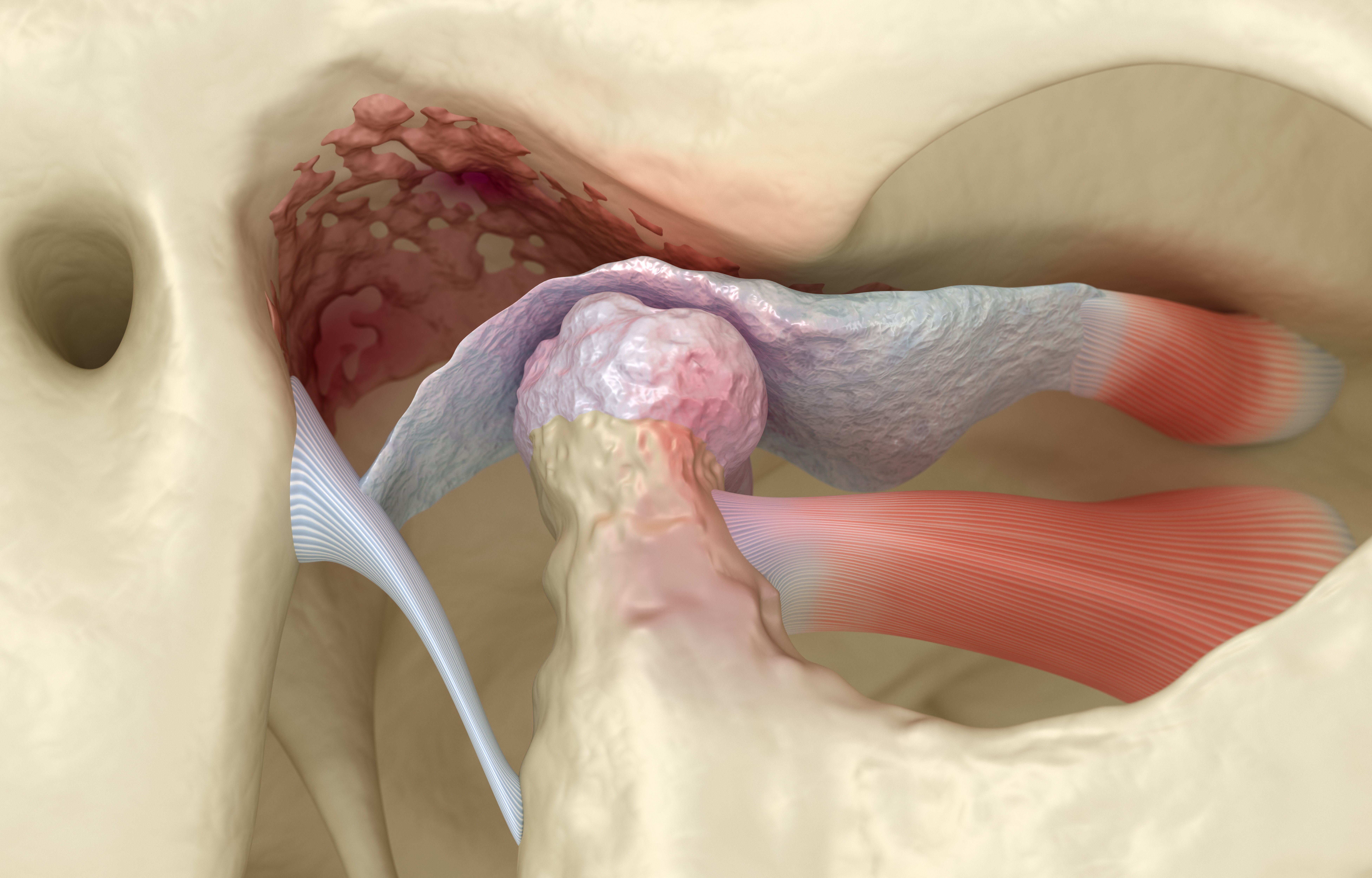 Platelet-Rich Fibrin (PRF) injections are minimally invasive treatment options for TMJ disorders and other orofacial pain conditions. PRF is the latest 2nd generation Platelet Concentrate that utilizes your own blood to release natural growth factors and promote natural healing and tissue regeneration, including helping to heal the TMJ disc. The treatment involves collecting a sample of blood from the patient and processing it in Special Centrifuges made for PRF to separate out the platelets and fibrin, which are then re-injected into the treatment area. The platelets in PRF contain growth factors that help to stimulate the body’s natural healing processes, including TMJ Disc and surrounding Joint complex while the fibrin helps to create a scaffold for new tissue to grow on.
Platelet-Rich Fibrin (PRF) injections are minimally invasive treatment options for TMJ disorders and other orofacial pain conditions. PRF is the latest 2nd generation Platelet Concentrate that utilizes your own blood to release natural growth factors and promote natural healing and tissue regeneration, including helping to heal the TMJ disc. The treatment involves collecting a sample of blood from the patient and processing it in Special Centrifuges made for PRF to separate out the platelets and fibrin, which are then re-injected into the treatment area. The platelets in PRF contain growth factors that help to stimulate the body’s natural healing processes, including TMJ Disc and surrounding Joint complex while the fibrin helps to create a scaffold for new tissue to grow on.
Numerous clinical studies have shown that PRF treatment can be effective in promoting healing and tissue regeneration, and it is considered a safe and effective procedure. We utilize PRF in the TMJ to encourage healing, prevent arthritis, and reduce inflammation.
Hyaluronic Acid a.k.a. Visco Supplementation:
This may be a treatment option for TMJ inflammation, degeneration, or reduced lubrication.
Proliferation Injection Therapy a.k.a. Prolotherapy:
This injection is a combination of dextrose or saline, a local anesthetic which helps stabilize the TMJ, improves its range of motion, helps prevent dislocation in a hypermobile joint, and also relieves pain.
Biofeedback Therapy
Biofeedback therapy of TMJ involves the use of sensitive electronic instrumentation to monitor and provide real-time physiological data, encompassing parameters such as heart rate, muscle tension, and peripheral skin temperature. This therapeutic modality has demonstrated clinical efficacy in the management of various pain syndromes, including but not limited to orofacial pain, migraines, and tension-type headaches. Furthermore, biofeedback is an effective intervention for addressing comorbid conditions such as anxiety and stress, which frequently contribute to or exacerbate pain symptomatology.
Photobiomodulation
Photobiomodulation (PBM), also known as red light or low-level laser therapy, is a non-invasive treatment for Temporomandibular Joint (TMJ) disorders. PBM uses specific wavelengths of light to reduce inflammation, stimulate cellular repair, and alleviate pain, improving jaw function and overall well-being for individuals with TMJ issues.
Transcutaneous Electrical Nerve Stimulation (TENS)
TENS therapy is a non-invasive neuromodulation technique employed for pain management. This therapeutic modality involves the transdermal application of pulsed biphasic electrical currents via surface electrodes. The underlying mechanism of TENS-induced analgesia is hypothesized to involve both gating mechanisms within the spinal cord and the release of endogenous opioids, thereby mitigating nociceptive signal transmission. TENS is recognized for its favorable safety profile and rapid onset of pain attenuation, circumventing the systemic adverse effects associated with pharmacological interventions.
There are many other adjunctive care treatments to manage TMJ disorders. We focus on both pain relief and proactive management of your TMJ, utilizing non-surgical therapies to limit further deterioration of the joint(s).
However, for some patients whose TMJ disorder in one or both joints have significantly progressed before diagnosis, surgical interventions such as TMJ arthroscopy, arthrocentesis, or single/both TMJ replacement may be required as a final option.
With our rigorous specialized clinical training in TMJ disorders, we routinely work with TMJ/Oral and Maxillofacial surgeons to manage complicated cases before and after surgeries.
