Orofacial Pain, TMJ Disorders & Dental Sleep Medicine Specialists
Healing the Source, Not Just the SymptomsOrofacial Pain
Orofacial Pain (OFP) is one of the specialties in dentistry recognized by the American Dental Association that encompasses the diagnosis, management, and treatment of pain disorders of the jaw, mouth, face, head, and neck. The specialty of Orofacial Pain is dedicated to the evidenced-based understanding of the underlying pathophysiology, etiology, prevention, and treatment of these disorders and improving access to interdisciplinary patient care.
The American Academy of Orofacial Pain (AAOP) was founded in 1975 as a professional member organization. The AAOP is a scientific community of about 500 professionals in the United States with an interest in Orofacial Pain.
Orofacial Pain associated disorders include, but are not limited to, temporomandibular muscle and joint disorders, jaw movement disorders, neuropathic and neurovascular pain disorders, headache, and sleep disorders. Symptoms may include atypical pains or sensations such as ringing in the ears (tinnitus), dizziness, muscular incoordination, or even abnormal itching or tingling in the head and neck region.

Conditions We Routinely Treat
- Orofacial Pain
- Myofascial pain and other masticatory muscle disorders
- Atypical Facial Pain
- Headaches, Migraines, or Cluster Headaches
- Painful Post-Traumatic Trigeminal Neuropathy
- Trigeminal Neuralgia
- Cephalic/Cranial/Glossopharyngeal/Occipital neuralgias
- Orofacial Dyskinesia
- Odontogenic/Dental Pain
- Burning Mouth Syndrome
TMJ Disorders/TMD
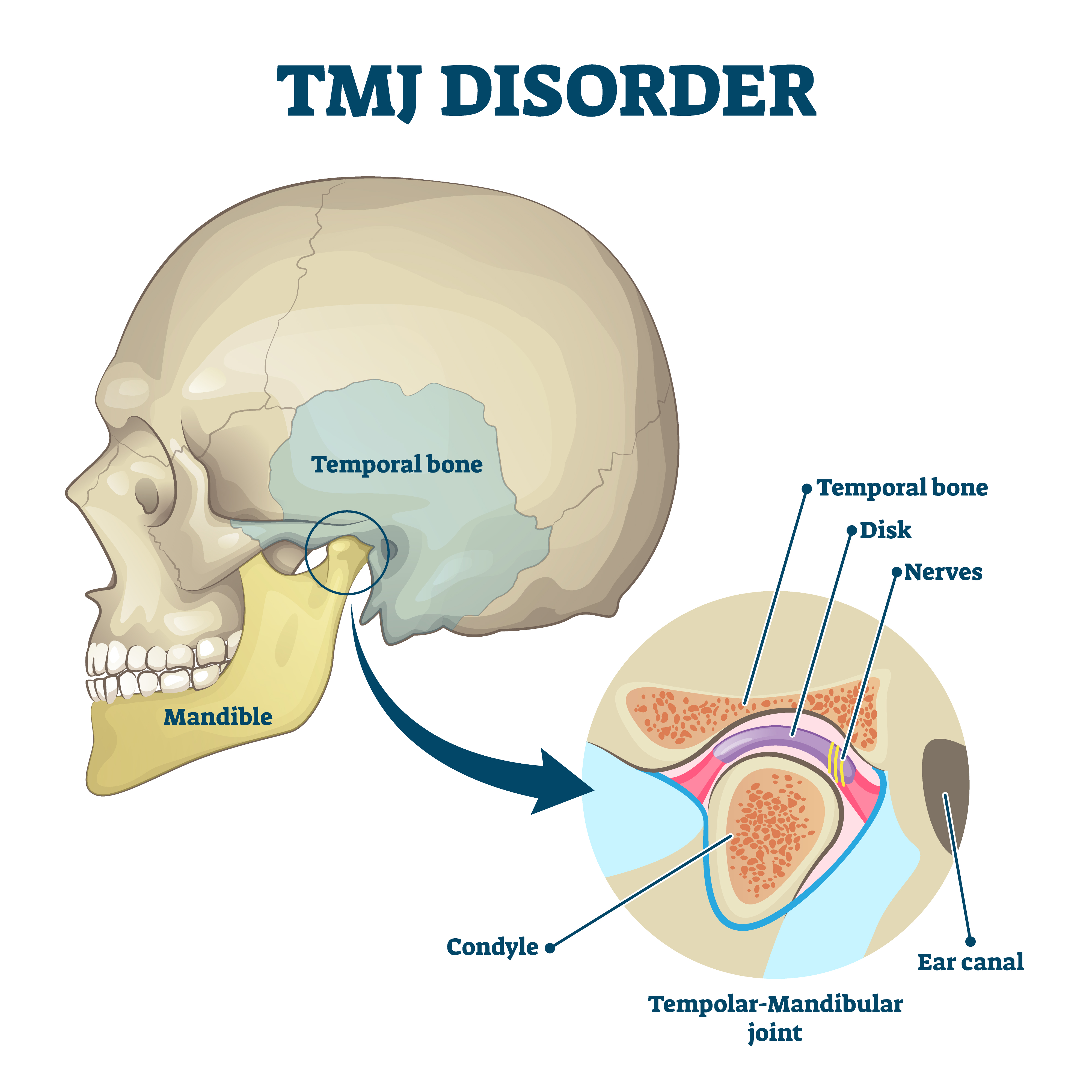
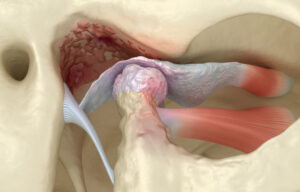
TMJ stands for Temporomandibular Joint, TMD is Temporomandibular Joint Disorders. The Temporomandibular Joint (TMJ) Association states that estimates range from 10 million to over 35 million people in the United States are affected by TMJ disorders (TMDs) at any given time.
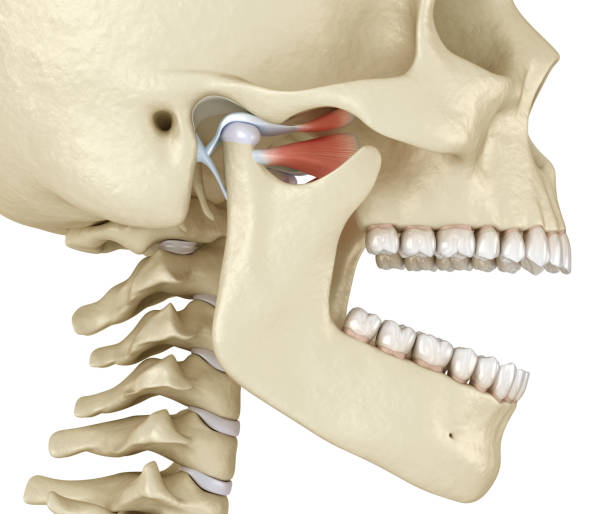
The temporomandibular joint is one of the most active joints in the body. It is involved in a wide range of daily activities, and as such, it gets used a lot. Estimates vary slightly, but generally, a person uses their TMJ between 2,000 and 3,000 times per day.
Understanding TMJ Disorders
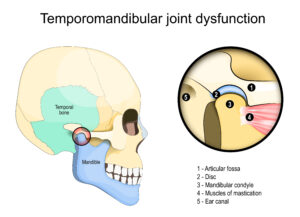
Temporomandibular Joint Disorder (TMD) is a complex condition that affects the jaw joint and surrounding muscles. The lower jawbone (mandible) and the temporal bone of the skull are connected by the temporomandibular joint (TMJ), which acts as a hinge. These joints control jaw movement and are situated on both sides of the head, just in front of each ear. They collaborate with muscles to do so. They enable essential functions like chewing, talking, and opening and closing the mouth.
TMD is a condition in which one or both joints are dysfunctional. This can be caused by structural problems, muscle problems, or lifestyle factors. The disorder affects the muscles and joints that move, causing pain and discomfort. While mild cases may resolve on their own, more severe or persistent TMD often requires professional treatment to manage symptoms and restore proper jaw function.
Routinely, jaw movements include chewing, talking, yawning as well as mouth breathing and snoring. The National Institute of Health estimates 10 million Americans are afflicted with some form of TMD that is capable of developing into significant, long-term problems.
TMJ Conditions We Routinely Treat:
- Headaches, earaches, and facial discomfort due to TMJ disorders
- Crunchy sensations or jaw dislocation
- Clicking, popping, crunchy or cracking sounds in the jaw
- Jaw locking or difficulty opening/closing the mouth
- Pain or tenderness in the jaw, face, or around the ears
- Ringing, fullness, or hearing loss in one or both ears
- Degenerative Joint Disease of one or both sides
The temporomandibular joint is one of the most active joints in the body. It is involved in a wide range of daily activities, and as such, it gets used a lot. Estimates vary slightly, but generally, a person uses their TMJ between 2,000 and 3,000 times per day.
Temporomandibular Joint Disorder (TMD) is a complex condition that affects the jaw joint and surrounding muscles. The lower jawbone (mandible) and the temporal bone of the skull are connected by the temporomandibular joint (TMJ), which acts as a hinge. These joints control jaw movement and are situated on both sides of the head, just in front of each ear. They collaborate with muscles to do so. They enable essential functions like chewing, talking, and opening and closing the mouth.
TMD is a condition in which one or both joints are dysfunctional. This can be caused by structural problems, muscle problems, or lifestyle factors. The disorder affects the muscles and joints that move, causing pain and discomfort. While mild cases may resolve on their own, more severe or persistent TMD often requires professional treatment to manage symptoms and restore proper jaw function.
Routinely, jaw movements include chewing, talking, yawning as well as mouth breathing and snoring. The National Institute of Health estimates 10 million Americans are afflicted with some form of TMD that is capable of developing into significant, long-term problems.
The prevalence of TMD is estimated to be between 5% and 12% of the population. A systematic review and meta-analysis found an overall prevalence of approximately 31% for adults/elderly.
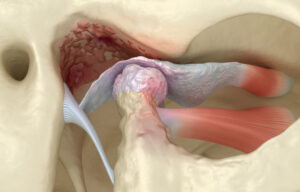
People suffering from TMD usually have symptoms that include clicking, popping, dislocating, cracking, crunchy sounds in the TMJ area, or jaw locking. This may be due to the TMJ disc that cushions the joint and might be dislocating or getting stuck. Sometimes people complain of ringing/fullness in one or both ears and may experience hearing loss.
“I used to hear clicking in my TMJ, and now I don’t. What does that mean?”
It’s common for patients to notice changes in their jaw sounds over time. If you used to experience a “clicking” sound when opening or closing your mouth and it has now stopped, it can indicate a few different things regarding your TMJ discs:

We understand why you might think that since the clicking has stopped, the problem has resolved. However, it’s important to understand why continued evaluation is often recommended:
Botulinum Toxin Injection, e.g., Botox/Xeomin: For relaxation of overactive muscles to reduce clenching and/or grinding and to alleviate pain.
Collaborative Approach

When Clicking Stops: What Does It Mean?
It’s common for patients to notice changes in their jaw sounds over time. If you used to experience a “clicking” sound when opening or closing your mouth and it has now stopped, it can indicate a few different things regarding your TMJ discs:
- Positive Change (Mild Cases): In some instances, the clicking may have stopped because the disc, which acts as a cushion between the bones of your jaw joint, has successfully returned to its proper, stable position. This means the disc is no longer slipping back and forth, and your joint mechanics have improved.
- A Shift in Disc Position (More Significant Cases): Alternatively, the cessation of clicking can sometimes mean that the disc has now fully displaced and is no longer moving in and out of place to create the sound. While the clicking has stopped, the disc may no longer be properly positioned between the bones of the joint.
TMJ/TMD Management Options
Advanced Injection Therapies
Trigger Point Injections
Injecting medication to break the muscle knots in your jaw muscles.
Botulinum Toxin Injection (e.g., Botox)
For relaxation of overactive muscles to reduce clenching and/or grinding and to alleviate pain.
Regenerative Injection Therapies
Platelet-Rich Fibrin (PRF)
PRF injections are minimally invasive treatment options for TMJ disorders and other orofacial pain conditions. PRF is a second-generation platelet concentrate that utilizes your own blood to release natural growth factors and promote natural healing and tissue regeneration, including helping to heal the TMJ disc. The treatment involves collecting a sample of blood from the patient and processing it to separate out the platelets and fibrin, which are then re-injected into the treatment area.
The platelets in PRF contain growth factors that help to stimulate the body’s natural healing processes, while the fibrin helps to create a scaffold for new tissue to grow on.
Numerous clinical studies have shown that PRF treatment can be effective in promoting healing and tissue regeneration, and it is considered a safe and effective procedure. We utilize PRF in the TMJ to encourage healing, prevent arthritis, and reduce inflammation.
Hyaluronic Acid (Visco Supplementation)
This may be a treatment option for TMJ inflammation, degeneration, or reduced lubrication.
Proliferation Injection Therapy (Prolotherapy)
This injection is a combination of dextrose or saline, a local anesthetic which helps stabilize the TMJ, improves its range of motion, helps prevent dislocation in a hypermobile joint, and also relieves pain.
Additional Therapies
We focus on both pain relief and proactive management of your TMJ, utilizing non-surgical therapies to limit further deterioration of the joint(s).
However, for some patients whose TMJ disorder in one or both joints has significantly progressed before diagnosis, surgical interventions such as TMJ arthroscopy, arthrocentesis, or single/both TMJ replacement may be required as a final option. With our rigorous specialized training in TMJ disorders, we routinely work with TMJ/Oral and Maxillofacial surgeons to manage complicated cases before and after surgeries.
Sleep Apnea/Snoring Treatment
Snoring is a major cause of sleep deprivation. As one of the most common sleep disorders, sleep apnea can seriously affect your quality of life. Left untreated, sleep apnea’s hallmark symptoms of snoring and daytime sleepiness can turn into serious issues like high blood pressure, heart arrhythmias, heart attack, and stroke.
Are you feeling worn out from restless nights and those unsettling pauses in your breathing? You’ve landed in the right spot. We firmly believe everyone deserves truly restorative sleep!
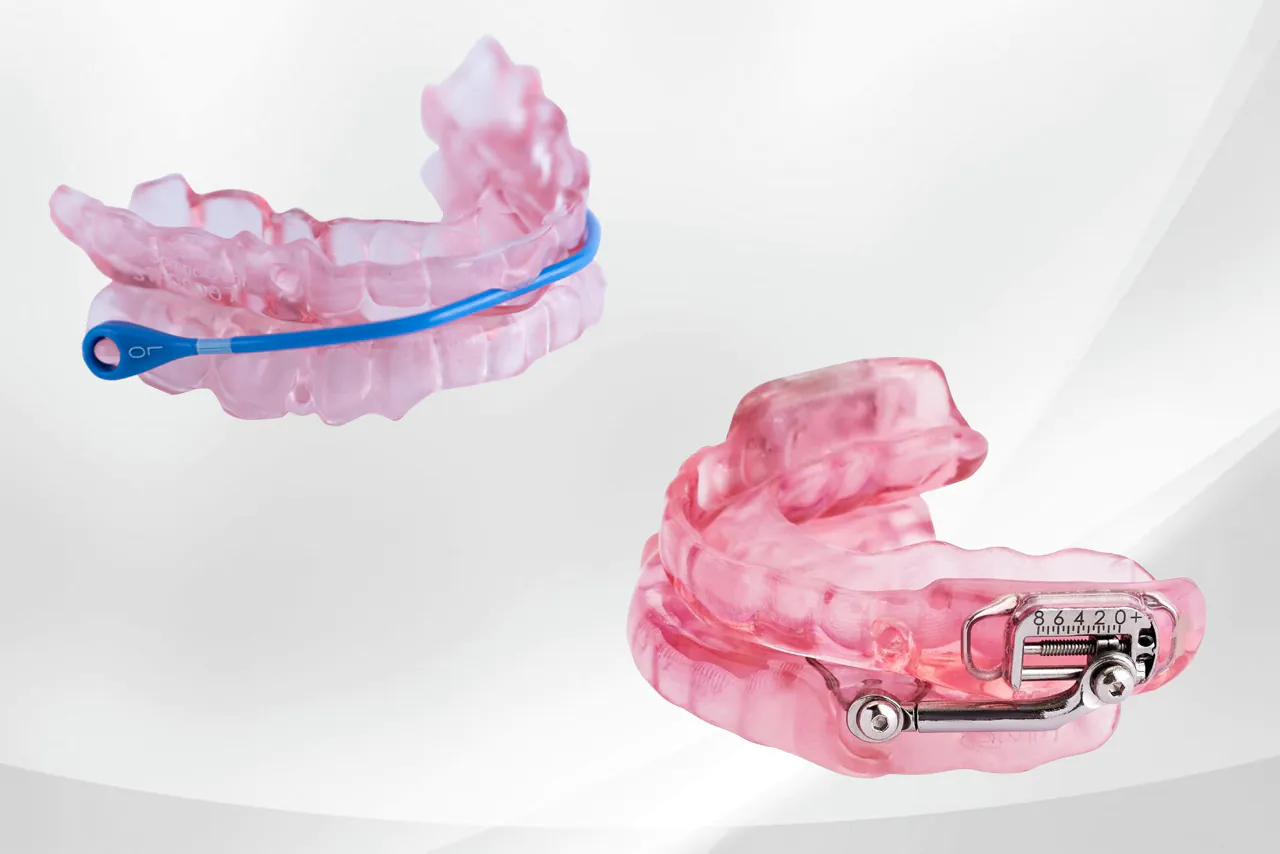
Whether you’re sick of feeling drained all day, constantly tired, or if your loved ones are complaining about your snoring, our oral appliances are designed to manage sleep-related breathing disorders. Our goal is to ensure you and your family can enjoy peaceful, uninterrupted sleep every single night.
Our Approach to Sleep Apnea
Ready to take control of your sleep?
Our specialists trained in Dental Sleep Medicine working in conjunction with sleep experts collaborate to diagnose sleep apnea and suggest treatments that can restore your sound and restful sleep. Snoring is a major factor in poor sleep quality/deprivation. Many people snore without even realizing it and this has the potential to be extremely disruptive to not only your sleep but also those around you.
A Collaborative Approach to Your Sleep Apnea
We believe in a multidisciplinary approach to managing your Obstructive Sleep Apnea (OSA), working closely with Pulmonologists and Sleep Specialists. Our goal is for you to experience better sleep, stop snoring, and wake up feeling refreshed. We’ll monitor your progress with follow-up sleep studies, which can be done conveniently at home (ordered over the phone) or, sometimes, in a sleep laboratory.
Effective, Convenient FDA approved Oral Devices
While clinical studies show the overall adherence rate for CPAP users is about 72%, we offer a different solution. We provide FDA-approved oral devices that can effectively manage your OSA. These devices are designed to last for years and, unlike a CPAP machine, don’t need to be plugged in — perfect for travelers, pilots, truck drivers, fellow campers, or anyone who values portability!
Why Treat Sleep Apnea?
- Improve sleep quality and daytime alertness
- Reduce risk of cardiovascular problems
- Enhance overall quality of life
- Benefit your partner’s sleep by reducing snoring
Ready to Improve Your Quality of Life?
Contact us today to schedule a consultation and learn more about our specialized services.
Contact Us